
New clinical trial for people with glioblastoma
Adaptive trial design allows scientists at UCSF, globally to rapidly evaluate more treatments
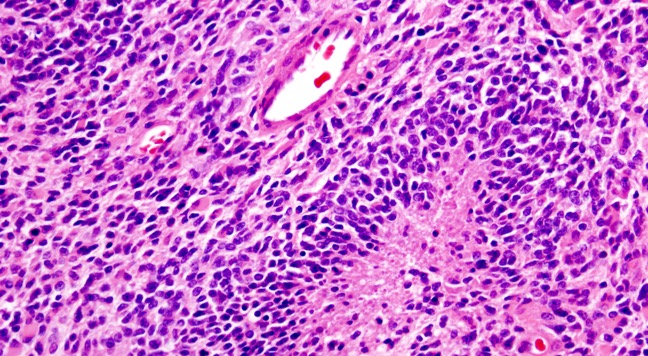
Patients with glioblastoma (GBM) have a poor prognosis, often not surviving longer than eighteen months.
A clinical trial for newly diagnosed and recurrent glioblastoma is opening for enrollment within the next couple of weeks at the UCSF Brain Tumor Center. This global Phase II/III trial will evaluate several different therapies in multiple treatment arms.
“Our goal in this trial is to rapidly identify effective therapies for GBM,” said chief of the Division of Neuro-Oncology within the Department of Neurological Surgery John de Groot, MD. “This would greatly expand the treatment armamentarium for our patients.”

The most established biomarker for GBM is called O-6 methyl guanine methyltransferase (MGMT). When MGMT is not modified by the cellular process called methylation, cancer patients tend to not respond well to standard treatments. Clinical trials for MGMT unmethylated GBM are designed to include novel agents in the place of temozolomide. GBM AGILE is evaluating multiple therapies to replace temozolomide in patients with newly diagnosed GBM with both methylated and unmethylated MGMT.
Scientists are aggressively developing new therapies including immunotherapies designed to enhance the immune system’s targeting of tumors, cell signaling pathway inhibitors block tumor growth, and cytotoxic chemotherapies that directly kill cancer cells. These novel therapies need to be evaluated in the clinical setting with a contemporary control arm to compare outcomes with standard approaches.
The multi-national trial UCSF is participating in, led by sponsor Global Coalition for Adaptive Research, takes an alternative approach to testing new treatments for GBM. Traditionally, researchers use a two-armed randomized and controlled clinical trial to evaluate a new therapies efficacy. However, this process is slow and only evaluates one new treatment at a time.
“The importance of a contemporary control arm cannot be over emphasized,” de Groot said. “Many therapies have been advanced into late-stage clinical trials after being inappropriately compared to older historical controls that do not accurately depict the real-life outcomes of patients.”
By using a statistical method called Bayesian adaptive randomization, scientists use real-time data during the trial to randomize patients into treatment arms that are statistically more effective. This increases enrollment of patients onto treatment arms that are more promising.
de Groot is the principal investigator for one of the treatment arms of the trial that involves a drug called VAL-083 that directly kills brain tumor cells. UCSF neuro-oncologist Nicholas Butowski, MD, is the UCSF principal investigator for the trial, which will recruit newly diagnosed and recurrent GBM patients at UCSF Health.
de Groot, who also sits on the Agent Selection Committee that determines whether an experimental therapy is eligible to be incorporated into a future clinical trial arms for the global trial, hopes the adaptive study design will help scientists more quickly understand whether a treatment is helping patients.
For More Information on Enrollment:
A Trial to Evaluate Multiple Regimens in Newly Diagnosed and Recurrent Glioblastoma (GBM AGILE)