Meningioma
A meningioma is a tumor that forms from the meninges, the name for the protective membrane layers surrounding the brain and spinal cord.
UCSF Medical Center is one of the only hospitals in the country with a dedicated comprehensive program for the treatment of meningiomas. Our multidisciplinary team includes experts across neurosurgery, neuro-oncology, radiation oncology, nursing, neuropathology, and neuroradiology. These experts meet weekly at a “tumor board” conference, where they work together to develop personalized treatment plans for each patient.
The meninges is composed of three protective layers called the dura mater, arachnoid mater, and pia mater. More specifically, meningiomas arise from cells in the middle meningeal layer, the arachnoid mater.
Most meningiomas are benign and slow growing, but some grow more quickly and are classified as higher grade.
- Grade 1 meningiomas are slow growing.
- Grade 2, or atypical, meningiomas grow more quickly and are more likely to recur. These tumor cells have more abnormalities than those in grade 1 meningiomas.
- Grade 3, or anaplastic, meningiomas are more aggressive, show more cellular abnormalities, often recur rapidly, and have a higher likelihood of invading surrounding normal brain tissue. Anaplastic meningiomas are relatively rare, accounting for 0.3% of meningiomas.1
Sometimes meningiomas may also be described based on their locations within the nervous system. A few of the more common locations for meningiomas are listed below:
- Convexity meningioma occurs on the surface of the brain under the skull and pushes inward on brain tissue as it grows.
- Parasagittal meningioma occurs near the midline of the brain that separates left and right cerebral hemispheres.
- Intraventricular meningioma occurs within the ventricular system, a series of fluid-filled cavities within the brain.
- Sphenoid ridge meningioma occurs near the bony ridge behind the eyes and nose.
- Skull base meningioma occurs near the bones in the bottom of the skull.
- Olfactory groove meningioma occurs near the olfactory (smell sensing) nerves, above the nose.
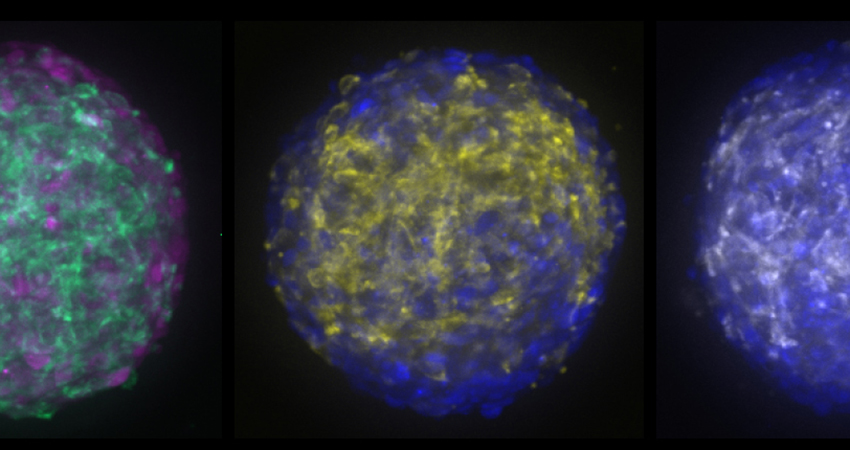
In addition, meningioma can be further described based on how the cells look under a microscope (its histological characteristics). Features that may distinguish these subtypes include the size and shape of the tumor cells. There are many histopathological subtypes described.
Symptoms of meningioma vary greatly depending on the size and location of the tumor. Most meningiomas are slow-growing and may not cause symptoms initially. Symptoms commonly arise when the tumor is large enough apply pressure on surrounding brain tissue, which can interfere with normal brain functions. Symptoms of meningioma may include the following:
- Headache
- Seizure
- Nausea or vomiting
- Personality changes
- Muscle weakness
- Vision problems
- Gait changes
Specific symptoms may relate to the location of the tumor, and the neighboring brain tissue that is being compressed. For example, intraventricular meningioma may block the flow of cerebrospinal fluid (CSF), which increases pressure in the brain and can cause headaches.
Sphenoid ridge meningioma may grow large enough to cause vision problems, or compress nearby cranial nerves, which may result in facial numbness.
Olfactory groove meningioma can result in loss of smell if the olfactory nerves are compressed; vision problems may even occur if the tumor is large enough to compress the optic nerves, which transmit information from the eyes to the brain.
Meningiomas are the most common type of brain tumor, and account for 41.7% of all primary brain tumors.1 From 2017-2021, an average of 39,059 cases of meningioma per year were reported in the United States.1 Meningiomas are most common in adults over 65 years and are also more commonly diagnosed in women.1
For most patients, the cause of meningioma is unknown. However, there are certain genetic conditions that may increase a patient’s chance of developing meningioma. For example, patients with neurofibromatosis type 2 (NF2) may be more likely to develop multiple and/or malignant meningiomas.2
Your personalized treatment plan may include surgery, drug therapy and/or radiation therapy.
The decision to operate on a tumor may depend on a variety of factors, including patient symptoms, age, and overall health. Depending on the size and location of the meningioma, surgery is the primary treatment for removal of the tumor. The objective is to remove as much of the tumor as possible, while preserving critical brain functions in the surrounding healthy tissue – this is called “maximal safe resection”. After surgery, each patient’s tumor tissue is analyzed with advanced genomic techniques to understand the molecular characteristics of the tumor. Together with traditional pathology, this information can give us a more accurate prognosis and identify treatment options that may be effective against the abnormalities present in your tumor.
For meningiomas that are small, slow-growing, and asymptomatic, doctors may suggest a period of observation with serial imaging scans before surgical or radiation therapies are considered.
Radiation therapy may also be used to treat meningiomas, especially in the case of inoperable tumors, or those that could not be fully removed during surgery. Advanced radiation techniques used may include IMRT or stereotactic radiosurgery (such as Gamma Knife) which both focus radiation beams in the tumor while minimizing exposure in surrounding healthy tissue.
For recurrent or more aggressive types of meningioma, there is no standard treatment. However, several ongoing research studies are investigating the use of chemotherapy (alone or in combination with radiation therapy) to treat these tumors.
Neurocognitive rehabilitation is also available through our Neurocognitive Care Services. Our multi-disciplinary team will assess each patient's needs, and devise an individualized plan to improve language, motor, or cognitive impairments caused by the brain tumor.
Overall, outcomes depend on the tumor grade, which may guide both treatment and prognosis. Many patients achieve excellent outcomes if the tumor can be completely removed surgically (which is called a “gross total resection”) or treated with radiation therapy. In patients where there is some tumor left behind (and even in some of those for whom the tumor is completely removed) tumor recurrence is possible. It is important to monitor meningiomas after treatment for recurrence.
Finding information about specific prognoses and survival rates is a personal decision. The current statistics are only summary data, and don’t necessarily reflect results from new or experimental therapies. These data do not determine how individual patients might respond to their treatment – everyone is different. That said, some people may choose to look for this information, which can be found in the most recent CBTRUS Statistical Report, in Tables 15-18.1
- Price M, et al. CBTRUS Statistical Report: Primary Brain and Other Central Nervous System Tumors Diagnosed in the United States in 2017-2021. Neuro Oncol, 2024;26(suppl_6): vi1-vi85.
- Campian, J. and D.H. Gutmann, CNS Tumors in Neurofibromatosis. J Clin Oncol, 2017. 35(21): p. 2378-2385.
Our Team
This content was reviewed by David Raleigh, MD, PhD.