Treatment Vaccines and Other Immunotherapy Trials Underway at UCSF
From genetically engineered viruses to antibody-based therapies, UCSF is currently investigating a number of novel immunotherapies for treating brain tumors. Several ongoing clinical trials are underway to evaluate immunotherapies for both adult and pediatric patients.
Immunotherapy encompasses a range of strategies aimed at making cancer cells more recognizable and vulnerable to attack by the patient’s immune system. "The goal is to identify immunotherapies that elicit a stable and effective immune response against tumor cells in the brain," said UCSF neuro-oncologist Nicholas Butowski, MD, who is leading several immunotherapy trials. "We are currently investigating the safety and efficacy of multiple immunotherapies, either alone or in combination with other treatment strategies."
Treatment Vaccines
Treatment vaccines are designed to help T cells recognize and target tumor cells, specifically those carrying certain mutations. This strategy takes advantage of mutations that exist in brain tumor cells, but not normal cells.
To create a treatment vaccine, synthetic molecules can be created in the lab to correspond to the mutated DNA sequence in a patient’s tumor. Alternatively, a treatment vaccine can be made from tumor lysate, a solution of ruptured tumor cells, which exposes the immune system to unique molecules made by the cancerous cells.
Once injected, the treatment vaccine will initiate an immune response that activates T-cells and antibodies. The T-cells and antibodies will then recognize, attack, and continually “remember” how to identify tumor cells based on the tumor-specific antigens in the vaccine.
UCSF is among the few institutions offering a clinical trial of personalized treatment vaccines for low-grade glioma in adults, as well as pediatric gliomas like DIPG:
- Neo-adjuvant Evaluation of Glioma Lysate Vaccines in WHO Grade II Glioma
- A Study of Varlilumab and IMA950 Vaccine Plus Poly-ICLC in Patients With WHO Grade II Low-Grade Glioma (LGG)
- H3.3K27M Peptide Vaccine for Children With Newly Diagnosed DIPG and Other Gliomas
Engineered Viruses and DNA Plasmids
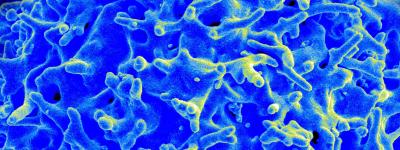
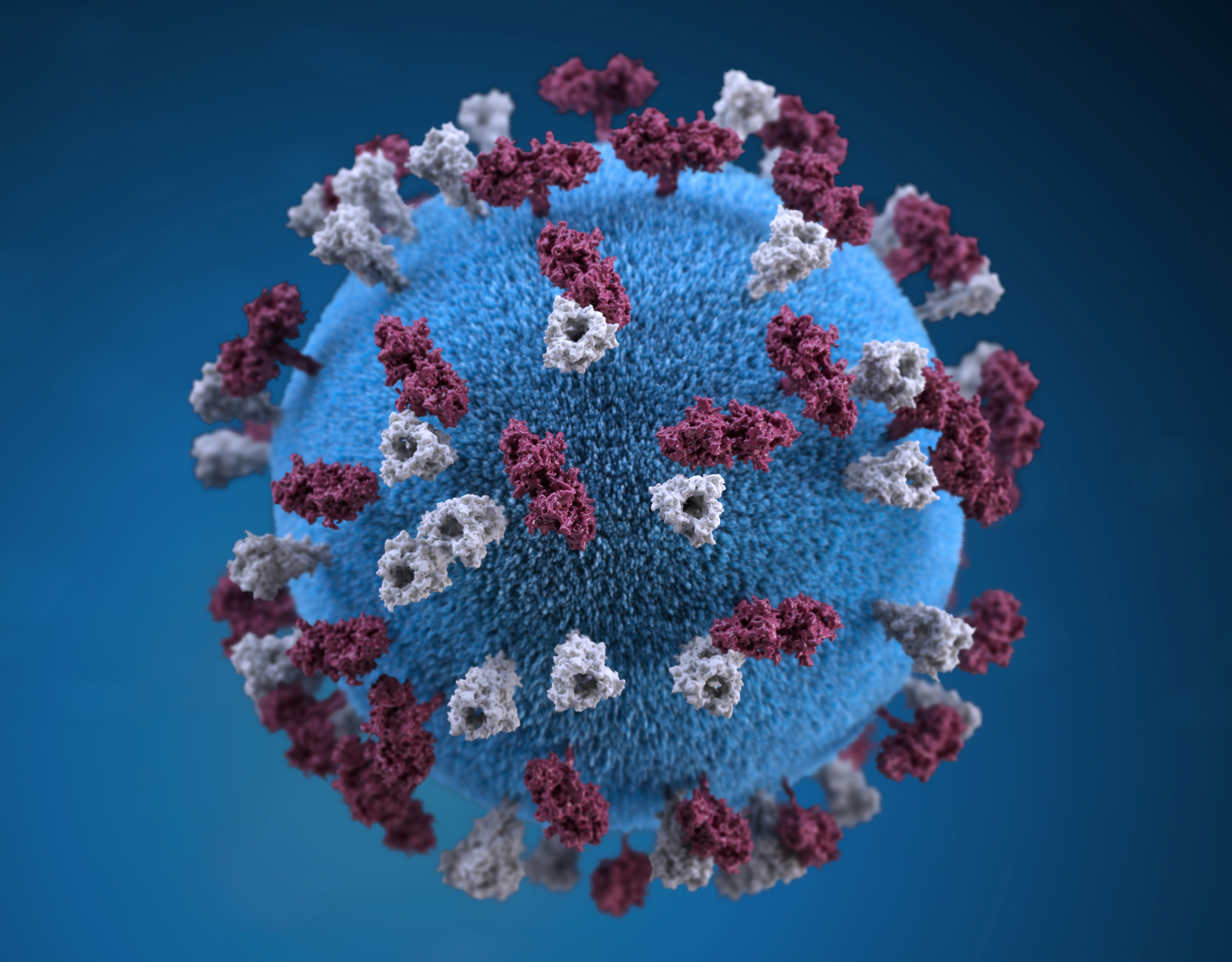
Some treatments use genetically engineered viruses that are no longer pathogenic or disease causing to normal cells. Instead the viruses are used to 1) deliver specific genes to certain cells, causing them to make those proteins, or 2) target and kill cancer cells.
For example, Ad-RTS-hIL-12 is an engineered virus that encodes the IL-12 protein and increases its production in specific cells. This is considered an immunotherapy treatment because IL-12 is a protein that may enhance the ability of the immune system to kill tumor cells. In some cases, engineered bacterial plasmids, or DNA molecules, may be used instead of viruses to deliver genes to cancer cells.
Engineered viruses can also be designed to specifically infect and kill tumor cells without harming healthy cells. These viruses, also called oncolytic viruses, infect cancer cells and multiply within them until the cell bursts. In bursting, the tumor cell releases molecules called tumor antigens, which allows the immune system to recognize and target remaining tumor cells.
UCSF offers a number of immunotherapies that involve engineered viruses or DNA plasmids, including oncolytic virus therapies. Ongoing clinical trials are assessing treatments for high-grade glioma in adults, as well as DIPG, medulloblastoma, and AT/RT in children:
- A Randomized, Multicenter, Phase 2 Study of Oncolytic Polio/Rhinovirus Recombinant (PVSRIPO) Alone or in Combination with Lomustine in Recurrent WHO Grade IV Malignant Glioma Patients
- A Phase I Study of Ad-RTS-hIL-12, an Inducible Adenoviral Vector Engineered to Express hIL-12 in the Presence of the Activator Ligand Veledimex in Pediatric Brain Tumor Subjects
- Modified Measles Virus (MV-NIS) for Children and Young Adults With Recurrent Medulloblastoma or Recurrent ATRT
Immune Checkpoint Inhibitors
Immune checkpoint inhibitors are a class of drugs that help block regulatory mechanisms that normally prevent the immune system from being overactive.
For example, several drugs are designed to block PD-1, a protein that normally protects the body from attacking itself. Normally, PD-1 works by detecting a molecular signal (called PDL-1) made by various cells across the body. Some cancer cells take advantage of this protection mechanism making the protective signal themselves. Blocking PD-1 with drugs like pembrolizumab or nivolumab allows the immune system to activate its T-cells and recognize these tumors as cells that should be attacked.
Pembrolizumab and nivolumab are also considered antibody-based therapies. Antibody-based therapies utilize antibodies that are designed to bind to specific molecules in the body. In this case, these two drugs bind and block PD-1, an immune checkpoint protein. Other antibody-based therapies target proteins that are enriched in tumors to 1) directly kill cancer cells or 2) ‘tag’ them so that the immune system can recognize and destroy them.
At UCSF, there are several ongoing clinical trials investigating use of immune checkpoint inhibitors, either alone or in combination with other therapies like radiation. We are currently evaluating these immunotherapies for treating adults with high-grade glioma, as well as children with DIPG and other advanced, relapsed, or refractory pediatric tumors:
- Pembrolizumab (MK-3475) in Patients With Recurrent Malignant Glioma With a Hypermutator Phenotype
- REGN2810 in Pediatric Patients With Relapsed, Refractory Solid, or Central Nervous System (CNS) Tumors and Safety and Efficacy of REGN2810 in Combination With Radiotherapy in Pediatric Patients With Newly Diagnosed or Recurrent Glioma
- A Study of Pembrolizumab (MK-3475) in Pediatric Participants With an Advanced Solid Tumor or Lymphoma
CAR and TCR Therapies
UCSF researchers in the Okada and Diaz Labs, are working to develop novel CAR T-cell therapies and T-cell receptor (TCR) therapies for adults and children with brain tumors.
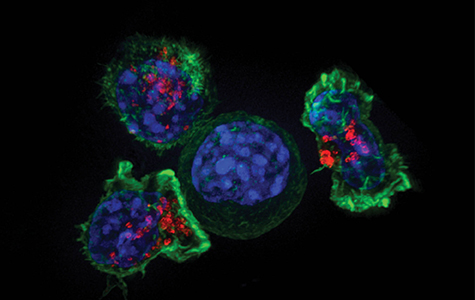
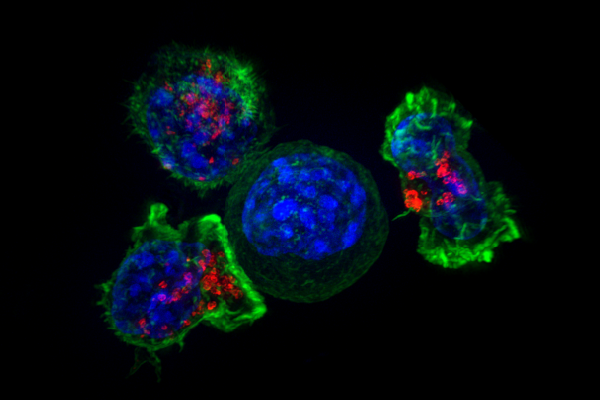
CAR and TCR therapies are both immunotherapies in which the patient's own T-cells are extracted from blood or tumor samples and genetically modified to better recognize and attack tumor cells. The modified T-cells are engineered to express special receptors that recognize molecules that are either enriched in or unique to tumor cells. After a growth period in the lab, millions of modified T-cells are then returned to the patient to help their immune system fight the tumor.
Browse the complete list of adult and pediatric clinical trials currently offered at UCSF.